Case Report #1
This will be the first case report. Thanks to Evan for the case. I'll try to provide these in a format that allows you to review the H&P, objective data and then provide some questions with regards to clinical decision making. I'll then provide the diagnosis followed by some learning bullets about the specific case. Ergo, I will withhold some information to allow you to think about the case a bit (ala oral boards). If you have any cases that you think we would be beneficial from a learning standpoint please give me the name and medical record number. These cases can be as simple an interesting x-ray, CT or EKG. The more cases you provide, the more I can put on the site and we all benefit.
I'm still working on some format issues. I don't want the EKG's to be on the top of the blog, but for time being consider the first one to be EKG #1 and the 2nd #2. And now on to case report #1...
CC: "Depressed"
HPI: 76 yo male depressed over a recent diagnosis of dementia. He denies any significant findings on ROS except for depression.
PMHx: Dementia, depression, CAD, HTN, hypercholesterolemia
Meds: Exelon, Triamterene, Digoxin, Lisinopril, Namenda, Pentoxifyline, Zocor
PSHx: CABG x 2
SHx: Denies tobacco or drugs. Rare alcohol use
ROS: Negative for all major systems except depression
V/S: Temp: 98 HR: 78 RR: 18 BP: 167/73 Sats: 98% (RA)
PE: No significant findings except for cardiovascular exam that reveals a bradycardic, irregularly irregular rhythm. Neuro exam non-focal. No other significant findings.
Question #1: Assuming this patient has no history of A-fib, what are some possible etiologies of his new A-fib?
Question #2: If this patient told you he was depressed and took extra medicine, which ones could cause potentially cause the new A-fib?
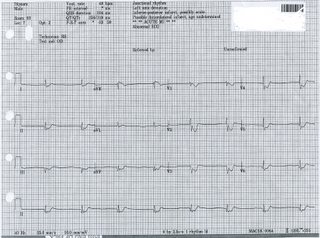
EKG #1:
An OD panel, cardiac markers and digoxin level were ordered.
Question #3: What are some signs and symptoms of digoxin toxicity?
Question #4: What EKG findings are consistent with digoxin toxicity?
Question #5: What are the criteria for administering Digibind?
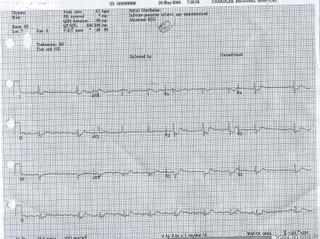
The patient was placed on a monitor with a HR of 61. He continued to become more bradycardic. A second EKG was performed.
EKG #2:
Significant lab values included a potassium of 4.8, creatinine of 1.1, ASA, tylenol and EtOH were all negative. The patients digoxin level was 35. The patient admitted to taking #8-10 Exelon 3 mg tablets and #16 Digoxin 0.125 mg tablets two hours PTA. A repeat potassium increased to 5.6. Toxicology was involved early and often. Digibind was appropriately administered and the patient was admitted to the ICU. He later was discharged to a SNF after being cleared by psych.
Learning Points:
- Digoxin increases the force of myocardial contraction, thereby increasing cardiac output in patients with heart failure. It affects the Na/K+ pump (remember your biochem).
- In toxic doses, the disruption of the pump prevents transport of K+ into the cells, thus you can get toxic hyperkalemia.
- Digoxin also increases vagal activity and decreases sympathetic activity. This results in decreased conduction through the AV node.
- In digoxin toxicity, you can get both tachy- and bradycardias.
- Common digoxin arrhythmias include EVERYTHING, but pathognomonic are A-fib w/ slow ventricular rate, bidirectional V-tach, and atrial tachycardia w/ associated AV block.
- Remember as well that digoxin typically gives an ST depression/scooping in the V5-V6 leads "hockey-stick". This is seen even at therapeutic doses. It may help however, in the case of AMS and you don't have a medication list.
- As a practice, if any patient is on digoxin and they have any complaint that could possibly be due to digoxin toxicity, ALWAYS CHECK A LEVEL. Rarely does this get done in triage and many times I've had to hold a patient while this gets done. So it'd help if we got the word to the triage nurses to be ordering this (my personal opinion).
- The most common constitutional symptoms are nausea, fatigue, anorexia, and visual disturbances (blue-green halo - "Van Gough effect")
- The mean peak digoxin level after an oral dose is 2 hours with a range of 0.5-6 hours.
- In chronic toxicity, the potassium is actually usually low-normal, but high in acute toxicity.
- Digitalis is found in foxglove, oleander and lily of the valley. (Remember these when you get the altered child who may have been eating plants or people who make home-brewed teas).
- Patients who are on digoxin are typically also taking diuretics. In these cases they commonly have hypomagnesemia. Try replacing Mg2+ with 1-2 g IV over 2 minutes to help with ventricular dysrhythmias.
- Indications for Digibind:
- a) ventricular dysrhythmias
- b) Progressive and hemodynamically significant bradydysrhythmias unresponsive to atropine
c) Serum potassium greater than 5 mEq/L
d) Rapidly progressive rhythm disturbances or rising serum potassium
e) Coingestion of cardiotoxic drug as β-blockers, calcium channel blockers, or tricyclic antidepressants
f) Ingestion of plant known to contain cardiac glycosides plus severe dysrhythmias (rare)
g)Acute ingestion greater than 10 mg plus any one of factors 1 through 6 above - h) Steady-state serum digoxin greater than 6 ng/ml plus any one of factors 1 through 6 above
- There are several formulas for determining how many vials of Digibind you'll administer. My thought is you're not going to remember them (factors include weight, bioavailability -80%, etc). Realistically, you're going to be consulting toxicology anyways AND it's very expensive. Thus, they're going to tell you how much. You also may have to give several doses.
That's it for this first case. Let me know if you thought it was helpful and if you have any cases forward them on.

1 Comments:
s
Post a Comment
<< Home